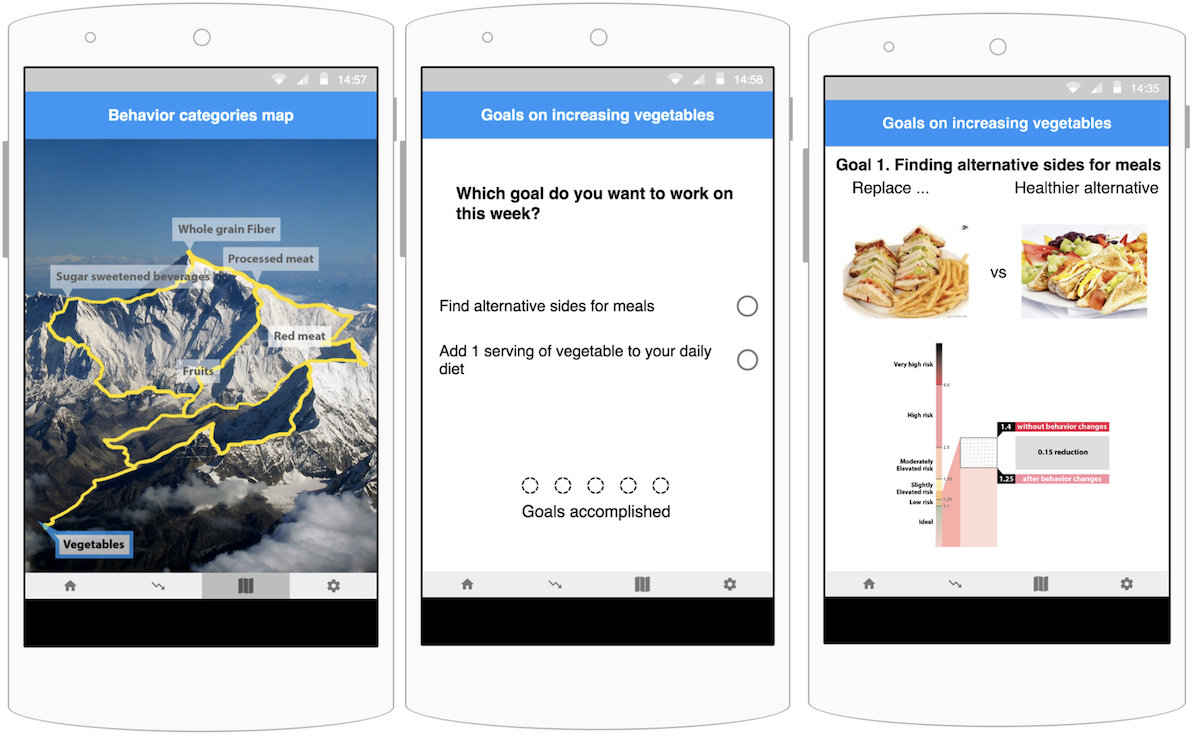
 Screens from the prototype presented to the focus group. Users can select which goal to work on using the mountain climbing metaphor (left). As users accomplish the goals, they can unlock the next category of goals. Selecting a category on the behavior category map will direct the user to the goal selection screen (center). The screen on the right shows choice for sides and how future cardiovascular risks might differ, if the user were to repeat the behavior for a week.
Screens from the prototype presented to the focus group. Users can select which goal to work on using the mountain climbing metaphor (left). As users accomplish the goals, they can unlock the next category of goals. Selecting a category on the behavior category map will direct the user to the goal selection screen (center). The screen on the right shows choice for sides and how future cardiovascular risks might differ, if the user were to repeat the behavior for a week.
Abstract
Background: Diet-tracking mobile apps have gained increased interest from both academic and clinical fields. However, quantity-focused diet tracking (eg, calorie counting) can be time-consuming and tedious, leading to unsustained adoption. Diet quality—focusing on high-quality dietary patterns rather than quantifying diet into calories—has shown effectiveness in improving heart disease risk. The Healthy Heart Score (HHS) predicts 20-year cardiovascular risks based on the consumption of foods from quality-focused food categories, rather than detailed serving sizes. No studies have examined how mobile health (mHealth) apps focusing on diet quality can bring promising results in health outcomes and ease of adoption. Objective: This study aims to design a mobile app to support the HHS-informed quality-focused dietary approach by enabling users to log simplified diet quality and view its real-time impact on future heart disease risks. Users were asked to log food categories that are the main predictors of the HHS. We measured the app’s feasibility and efficacy in improving individuals’ clinical and behavioral factors that affect future heart disease risks and app use. Methods: We recruited 38 participants who were overweight or obese with high heart disease risk and who used the app for 5 weeks and measured weight, blood sugar, blood pressure, HHS, and diet score (DS)—the measurement for diet quality—at baseline and week 5 of the intervention. Results: Most participants (30/38, 79%) used the app every week and showed significant improvements in DS (baseline: mean 1.31, SD 1.14; week 5: mean 2.36, SD 2.48; 2-tailed t test t29=−2.85; P=.008) and HHS (baseline: mean 22.94, SD 18.86; week 4: mean 22.15, SD 18.58; t29=2.41; P=.02) at week 5, although only 10 participants (10/38, 26%) checked their HHS risk scores more than once. Other outcomes, including weight, blood sugar, and blood pressure, did not show significant changes. Conclusions: Our study showed that our logging tool significantly improved dietary choices. Participants were not interested in seeing the HHS and perceived logging diet categories irrelevant to improving the HHS as important. We discuss the complexities of addressing health risks and quantity- versus quality-based health monitoring and incorporating secondary behavior change goals that matter to users when designing mHealth apps.